What Causes Nerve Damage in the Feet?
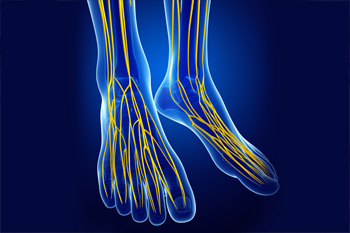
Peripheral neuropathy, a type of nerve damage that affects the extremities, is a complication associated with several diseases. One of the most common types of neuropathy is diabetic neuropathy. As its name suggests, this type of nerve damage occurs in people who have diabetes. Approximately 25% of diabetics have experienced pain caused by nerve damage. Other potential causes of peripheral neuropathy include vitamin deficiencies, alcohol abuse, foot injuries, hypothyroidism, kidney disease, Charcot-Marie-Tooth disease, and certain infections. Since neuropathy in the feet can cause a reduction or loss of sensation, the feet are at an increased risk of developing wounds, which may become infected. If you have peripheral neuropathy, it is suggested that you be under the care of a podiatrist.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Cory Brown, DPM from Cory Brown, DPM. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Healthy Weight Equals Happy Feet
 Individuals with a body mass index (BMI) that is more than 30 are considered to be obese. Obesity is believed to go hand in hand with certain foot disorders such as heel pain, tendonitis, arthritis, and other conditions caused from the stress of excess weight placed on the feet and ankles. Obesity can also put a person at risk for type II diabetes, which often leads to the development of other foot conditions. Losing weight can help reduce excess pressure on the feet and ankles, however exercising can be difficult when your feet are in pain. A podiatrist can treat foot conditions brought on by obesity and help alleviate foot pain by suggesting specific stretches and prescribing custom orthotics.
Individuals with a body mass index (BMI) that is more than 30 are considered to be obese. Obesity is believed to go hand in hand with certain foot disorders such as heel pain, tendonitis, arthritis, and other conditions caused from the stress of excess weight placed on the feet and ankles. Obesity can also put a person at risk for type II diabetes, which often leads to the development of other foot conditions. Losing weight can help reduce excess pressure on the feet and ankles, however exercising can be difficult when your feet are in pain. A podiatrist can treat foot conditions brought on by obesity and help alleviate foot pain by suggesting specific stretches and prescribing custom orthotics.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Obesity Affects Your Feet
Gaining weight can happen suddenly and at any time. Usually you won’t notice the extra weight until your feet start hurting at the end of the day. This happens as your feet begin adjusting to carrying more weight. Foot swelling and pain are two of the biggest side effects of having gained weight.
Many foot-related problems can occur even after just putting on a few pounds. This includes the body ‘compensating’ by changing the way it moves. You may find yourself putting extra weight on the wrong parts of your feet and even leaning forward a bit. Your feet were designed to carry a healthy, normal body weight. Extra weight places undue stress on them.
Being overweight often causes the development of Type-2 diabetes, causing leg and foot pain. Older people who do not attempt to control their condition can even lose sensation and feeling in their legs and feet. This can lead to the development of small sores that can lead to serious infection.
Extra stress placed on the joints, tendons and muscles in the feet as a result of extra body weight may also cause heel spurs, or plantar fasciitis. Plantar fasciitis is an inflammation of the foot tissue, causing stiffness and pain when walking and climbing stairs. This can usually be relieved by foot stretches and custom made orthotic shoe-inserts.
Problems in the feet triggered by obesity can be treated by paying special attention to footwear. Proper support shoes that allow for good circulation, especially in the arch and ankle, are vital. A podiatrist can help you find what sort of shoe is most suitable for your feet. They can also measure you for special orthotics if necessary.
It could also be high time to start losing weight in order to treat and prevent diabetes as well as other life threatening diseases. Some methods include yoga and water aerobics, which benefit your entire body without placing stress on your feet. Don’t risk losing your feet by losing interest in them. Take care of your feet and your body, as they deserve the very best.
Who Needs an ABI Test?
 An Ankle-Brachial Index (ABI) test is a screening tool that is used to assess circulation in the lower limbs. During an ABI test, the doctor takes your blood pressure at various points along your arms and lower legs and compares the numbers to determine your risk of having full or partial blockages in the blood flow of your lower limbs. Not everyone needs an ABI test. They are typically done for people who are at risk of peripheral artery disease, a condition characterized by poor circulation in the extremities. People who are at risk of having peripheral artery disease include those with a history of smoking, high blood pressure, high cholesterol, diabetes, and atherosclerosis, as well as older adults and people who have a family history of peripheral artery disease. To learn more, please consult with a podiatrist.
An Ankle-Brachial Index (ABI) test is a screening tool that is used to assess circulation in the lower limbs. During an ABI test, the doctor takes your blood pressure at various points along your arms and lower legs and compares the numbers to determine your risk of having full or partial blockages in the blood flow of your lower limbs. Not everyone needs an ABI test. They are typically done for people who are at risk of peripheral artery disease, a condition characterized by poor circulation in the extremities. People who are at risk of having peripheral artery disease include those with a history of smoking, high blood pressure, high cholesterol, diabetes, and atherosclerosis, as well as older adults and people who have a family history of peripheral artery disease. To learn more, please consult with a podiatrist.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with Cory Brown, DPM from Cory Brown, DPM. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Vascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.
Bursitis: A Real Pain in the Heel
There are many causes of heel pain, including bursitis. The retrocalcaneal bursa is a fluid-filled sac located between the heel bone and the Achilles tendon. It cushions and lubricates the tendon as it slides over the heel bone, while acting as a shock absorber during walking and other movements. Excessive walking, running, jumping or other stress inducing activities placed upon the ankle may cause this bursa to become swollen, irritated, and inflamed. The skin at the back of the heel may be warm or red. The affected area may also become very sensitive to the touch, and painful during physical activity or when standing on your toes. If you feel this type of pain at the back of your heel that does not improve with rest, it is in your best interest to schedule an appointment with a podiatrist. They will perform a physical examination and may recommend certain conservative treatments such as icing, anti-inflammatory medication, orthotics or heel wedges to reduce stress on the heel, ultrasound and/or physical therapy, or possibly even steroid injections if other methods do not work.
Many people suffer from bouts of heel pain. For more information, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.