What Are Diabetic Blisters?

Diabetic blisters are a common yet often overlooked complication of diabetes. These blisters typically appear on the feet and legs and are filled with clear fluid. They can be painless at first but may become sore or irritated if left untreated. Diabetic blisters are more likely to form due to poor circulation and nerve damage caused by high blood sugar levels, which makes the skin more fragile and susceptible to injury. While these blisters often heal on their own, they can become infected if not properly cared for. A podiatrist can help by properly cleaning and dressing the blister to reduce the risk of infection. This type of doctor may also advise on keeping the area protected and suggest ways to prevent further blisters. Additionally, a podiatrist may recommend custom footwear, or orthotics to reduce friction and pressure on the feet. If you have diabetes and have developed blisters, it is suggested that you are under the care of a podiatrist who can help you to manage this serious condition.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters on the Feet
Blisters are a common ailment of people who wear shoes that are either too tight or rub against the feet in an uncomfortable way. Knowing the basics of blisters is important for understanding how they are formed and what treatments should be used for them.
A blister on the foot, or any other part of the body, is a small pocket that is filled with fluid. It usually forms on the upper layer of the skin because these layers are loose enough to allow a blister to form. The most common fluid in a blister is just a clear, watery-like fluid that usually isn’t cause for concern. However, blisters can fill up with blood if they are deep enough and pus if they have become infected with bacteria.
Blisters almost always form on the feet due to shoes rubbing up against the foot, where the friction causes blisters. These can occur after you have walked for a long period of time or when your shoes do not fit you properly. Your feet are also more prone to blisters if they are moist, so keeping them dry and clean is one preventative step you can take.
Preventing infection should be the number one concern when treating blisters, as well as relieving the pain they can cause. Using a bandage to cover up the blister will help it heal and prevent bacteria from entering it. New skin will form under the blister and eventually cause it to pop. You can also take a sterilized pin and try to pop it yourself.
If the blister is filled with pus or blood, seeking treatment from a doctor is ideal. Antibiotics may need to be taken in order to completely eliminate the bacteria inside the blister. See a doctor to have an antibiotic prescribed.
The best way to treat blisters is to prevent them all together. Keeping your feet dry and making sure that your shoes fit properly are just two of the steps you can take to prevent blisters. Shoes that are too tight or shoes that are too loose and allow your feet to slide in them will cause blisters. Applying a bandage to an area where you think a blister is about to form is another way you can prevent them.
What to Know About Plantar Warts

Plantar warts, or verrucas, are common viral skin growths caused by the human papillomavirus, or HPV. They often appear on the soles of the feet, especially in children, athletes, and those with weakened immune systems. The virus thrives in warm, moist environments like near pools, and in locker rooms and communal showers, spreading through direct contact. These warts may look like thick, rough calluses with tiny black dots, which are clotted blood vessels and can cause pain when walking. Over time, they may spread or cluster into mosaic warts. Stubborn plantar warts can persist. If you or your child has a plantar wart, it is suggested that you see a podiatrist who can provide prescription medications, laser therapy, or minor surgical removal.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.
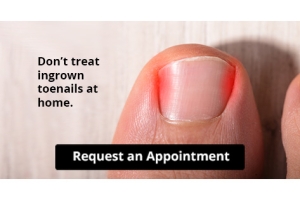
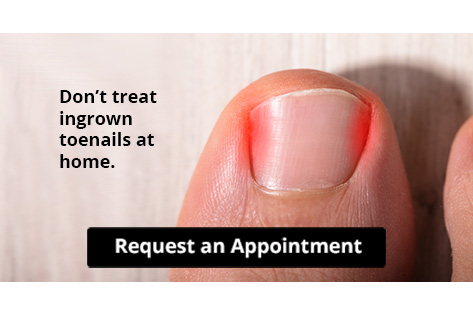
Let the Expert Treat Your Ingrown Toenails
Common Causes of Foot and Ankle Swelling

Foot and ankle swelling can occur for various reasons, often related to lifestyle, health conditions, or prolonged periods of immobility. One common cause is being overweight, as excess body weight places additional pressure on the feet and ankles, leading to fluid retention and swelling. Age is another factor, as older individuals may experience reduced circulation, which can contribute to swelling in the lower extremities. Leg infections can also cause swelling, as the body’s immune response leads to inflammation in the affected areas. Prolonged periods of immobility, such as on long airplane flights, can reduce circulation and lead to fluid buildup in the feet and ankles. A sedentary lifestyle, in which an individual remains seated or inactive for long stretches, can further cause swelling by preventing proper blood flow. If you have swollen feet or ankles, it is suggested that you confer with a podiatrist who can determine what the cause is, and offer appropriate treatment solutions.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
Causes and Treatment of Drop Foot

Drop foot, sometimes called foot drop, occurs when the muscles responsible for lifting the front part of the foot become weakened or paralyzed, making it difficult to walk without dragging the toes. Drop foot often leads to changes in gait, such as lifting the knee higher to avoid tripping. Causes of drop foot include nerve damage in the leg or spine, diabetes, or strokes. Symptoms may also involve numbness in the foot, loss of sensation, or a noticeable limp. Treatment by a podiatrist focuses on improving mobility and preventing further complications. Ankle-foot orthoses, or AFOs, can stabilize the foot and ankle, keeping the foot in a neutral position to reduce the risk of falls. Functional electrical stimulation may also be used to activate the muscles, improving walking patterns. A podiatrist can assess the underlying cause of drop foot and provide solutions to improve mobility and function. If you have symptoms of drop foot, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
If you have any concerns about your feet, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
Common Sources of Foot Pain

Foot pain affects many people due to the intricate structure of the foot and the stress it endures during daily activities. Bunions, caused by bone misalignment, can lead to discomfort and changes in foot shape. Deformities like claw toes and hammertoes, often linked to tight shoes or imbalanced muscles, can result in painful corns or calluses. Arthritis in the toes and ankles may cause stiffness and reduced mobility, with age and weight being contributing factors. Fractures from injuries, such as falls or missteps, and sprains from ligament damage can also be significant sources of pain. Conditions like athlete's foot, fungal infections, and nerve issues such as peripheral neuropathy, which causes tingling or burning sensations are other potential concerns. A podiatrist can evaluate any of these conditions and offer treatment ranging from orthotics for support to surgery, in more severe cases. If you have foot problems, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Cory Brown, DPM from Cory Brown, DPM. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.