Preventing Morton’s Neuroma
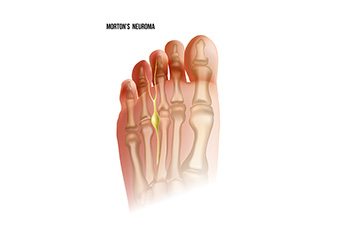
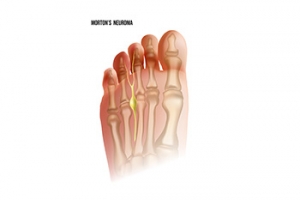
Plantar digital neuroma, commonly known as Morton's neuroma, is a painful condition involving the thickening of tissue surrounding one of the nerves leading to the toes. This condition typically develops between the third and fourth toes and causes sharp, burning pain and often a feeling of having a pebble in the shoe. Wearing high-heeled or tight shoes, repetitive stress, and certain foot deformities like bunions and hammertoes can contribute to developing a neuroma. To prevent plantar digital neuroma, it helps to wear well-fitted, low-heeled shoes with adequate toe room and cushioning. It is also beneficial to avoid activities that place excessive pressure on the ball of the foot. Regularly stretching, strengthening foot muscles, and maintaining a healthy weight can reduce the risk of Morton's neuroma. If you have pain between your toes, it is suggested that you consult a podiatrist who can accurately diagnose and treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Plantar Fibroma Excision Surgery

A sign a plantar fibroma has developed is a noticeable lump in the arch of the foot. If it becomes painful or uncomfortable, surgery may be considered. In plantar fibroma excision surgery, managing postoperative healing is critical. Closed incision negative pressure therapy, or CINPT, and surgical drain placement are two techniques used for this purpose. CINPT involves applying a sealed dressing connected to a vacuum pump, which continuously removes fluid and reduces edema, promoting faster healing and minimizing infection risk. This method maintains a sterile environment and can improve wound outcomes. On the other hand, surgical drain placement involves inserting a tube into the surgical site to remove fluid buildup. While effective in preventing hematoma or seroma formation, it requires careful monitoring and regular emptying. Drains can sometimes increase the risk of infection and discomfort. Choosing between CINPT and surgical drains depends on the specific needs of the patient and the podiatric surgeon’s preference, with CINPT often providing a more advanced and less invasive option for optimal healing. If you have a plantar fibroma that is causing you pain and discomfort, it is suggested that you consult a podiatrist who can determine which type of surgery is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Why Live with Pain and Numbness in Your Feet?
What Can Cause Cracked Heels?
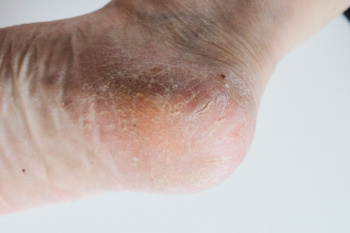
Cracked heels, a common foot ailment, can be caused by various factors. Vitamin deficiencies, particularly in vitamins A, C, and E, can lead to dry, flaky skin, making heels more prone to cracking. Excess weight gain places added pressure on the heels, leading to calluses and fissures. Wearing ill-fitting or open-back shoes exposes the heels to friction and pressure, exacerbating the problem. Additionally, genetics may also play a role, as some individuals naturally have drier skin or a predisposition to foot conditions. Unhygienic conditions, such as standing for long periods in damp environments or neglecting proper foot care, can contribute to cracked heels. Cracked heels can cause significant pain and discomfort. If this applies to you, it is strongly suggested that you confer with a podiatrist who can prescribe medication for effective relief.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Causes of Toenail Fungus
 Toenail fungus, also known as onychomycosis, is caused by a fungal infection. It can also be triggered by psoriasis, a chronic autoimmune skin disorder that affects the skin and nails, causing thickening, scaling, and inflammation. When psoriasis affects the nails, it can create pits, ridges, and discoloration, making them more likely to develop a fungal infection. Fungi thrive in warm, moist environments, such as sweaty socks and shoes. Additionally, fungi can be picked up by walking barefoot in communal spaces, such as locker rooms or swimming pool areas. Individuals with a weakened immune system, diabetes, or poor circulation are more likely to develop issues with toenail fungus. Injuries to the toenail, such as ongoing pressure or trauma, may provide opportunities for fungi to infect the nail bed. Practicing good foot hygiene, wearing breathable footwear, and avoiding walking barefoot in public areas can help prevent exposure to toenail fungus. If an infection occurs, it is suggested to seek prompt treatment from a podiatrist to prevent it from spreading and to restore the health of your toenails.
Toenail fungus, also known as onychomycosis, is caused by a fungal infection. It can also be triggered by psoriasis, a chronic autoimmune skin disorder that affects the skin and nails, causing thickening, scaling, and inflammation. When psoriasis affects the nails, it can create pits, ridges, and discoloration, making them more likely to develop a fungal infection. Fungi thrive in warm, moist environments, such as sweaty socks and shoes. Additionally, fungi can be picked up by walking barefoot in communal spaces, such as locker rooms or swimming pool areas. Individuals with a weakened immune system, diabetes, or poor circulation are more likely to develop issues with toenail fungus. Injuries to the toenail, such as ongoing pressure or trauma, may provide opportunities for fungi to infect the nail bed. Practicing good foot hygiene, wearing breathable footwear, and avoiding walking barefoot in public areas can help prevent exposure to toenail fungus. If an infection occurs, it is suggested to seek prompt treatment from a podiatrist to prevent it from spreading and to restore the health of your toenails.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Podiatrists Are Foot Health Specialists

A podiatrist, also known as a foot doctor, is a medical professional who specializes in diagnosing and treating conditions related to the feet, ankles, and lower extremities. Their primary focus is to ensure optimal foot health, addressing issues ranging from common ailments like bunions and ingrown toenails to complex conditions such as diabetic foot ulcers or sports injuries. In their workplace, podiatrists typically operate in clinics, hospitals, or private practices, equipped with diagnostic tools like X-rays and ultrasound machines. Podiatrists undergo extensive training, earning a Doctor of Podiatric Medicine, or DPM, degree from accredited podiatric medical schools. Some may further specialize in areas like sports medicine, wound care, or pediatric podiatry through postgraduate residencies or fellowships, honing their expertise to address specific patient needs effectively. If you are experiencing any type of foot condition, it is suggested that you consult a podiatrist who can offer you effective treatment solutions, in addition to answering any questions you may have about this field of medicine.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.