Items filtered by date: May 2025
Symptoms a Fractured Ankle

A broken ankle can occur when one or more of the bones in the ankle joint, which include the tibia, fibula, or talus, cracks or breaks due to a fall, collision, or twisting injury. Symptoms of a broken ankle include sudden and intense pain, swelling, bruising, and difficulty in moving the ankle. In many cases, walking becomes impossible, although some people may still bear weight, despite a fracture. A loud snapping sound may be heard at the time of injury. In more severe cases, the ankle may appear misshapen or the broken bone may pierce the skin. A podiatrist can examine the ankle for signs of damage and order imaging tests, such as X-rays, to confirm a fracture. Treatment depends on the location and severity of the break and may involve immobilization with a cast or surgery to realign the bones. Early diagnosis and treatment are important to reduce long-term complications. If you believe you may have fractured an ankle bone, it is suggested that you make an emergency appointment with a podiatrist for an exam and appropriate treatment.
Broken ankles need immediate treatment. If you are seeking treatment, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Get Professional Care for a Broken Foot or Ankle
Causes and Symptoms of Plantar Fasciitis
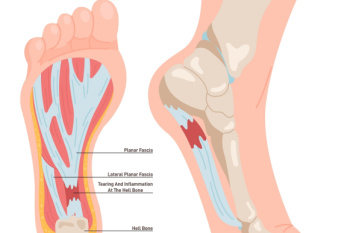
Plantar fasciitis occurs when the band of tissue that runs along the bottom of the foot, called the plantar fascia, becomes irritated or inflamed. This ligament supports the arch and absorbs pressure during walking. Repeated strain from activities like running, long periods of standing, or wearing shoes that lack proper support can lead to small tears where the fascia connects to the heel bone. Symptoms of plantar fasciitis often include sharp pain in the heel, especially with the first steps in the morning or after sitting for long periods. The pain may recede with movement but often returns later in the day. A podiatrist can diagnose plantar fasciitis by examining the foot and reviewing activity history. Treatment options include prescribed orthotics, anti-inflammatory medication, night splints, or, in some cases, corticosteroid injections. Surgery may be considered if other options fail. If you have pain on the bottom of your foot, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes and Treatment of Flat Feet

Flat feet occur when the arches of the feet are low or absent, causing the soles to make full contact with the ground while standing. Flat feet may be present from childhood or develop later from weakened tendons, ligament injuries, fractures, or arthritis. Some people with flat feet have no symptoms, but others experience aching in the arches, heels, ankles, or discomfort that extends to the knees and lower back. A podiatrist can diagnose flat feet by examining foot posture and gait, and may use imaging tests to evaluate the bones and soft tissues. When flat feet cause pain, medical treatment options include wearing custom orthotics or specially designed supportive footwear to reduce strain. In more severe cases, surgery may be recommended to strengthen or realign the affected structures in the feet. Early medical care can help manage symptoms and prevent further complications. If flat feet are disrupting your daily activities, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Cory Brown, DPM from Cory Brown, DPM. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors for Bunions

A bunion is a bony bump that forms at the base of the big toe as the top of the toe leans inward toward the others. This deformity develops over time due to pressure on the big toe joint, leading to changes in the bone structure. Common causes of bunions include wearing tight or narrow shoes, genetic predisposition, and conditions like arthritis that affect the joints. Risk factors include having a family history of bunions, flat feet, and occupations that involve long periods of standing or walking. Symptoms of a bunion often include swelling, redness, tenderness, and pain surrounding the big toe joint. Over time, the discomfort can worsen, making it difficult to wear shoes comfortably and affecting overall foot function. If you have a bunion, it is suggested that you are under the care of a podiatrist who can offer treatment options to manage this condition.
If you are suffering from bunion pain, contact Cory Brown, DPM of Cory Brown, DPM. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Lewiston, ID . We offer the newest diagnostic and treatment technologies for all your foot care needs.

